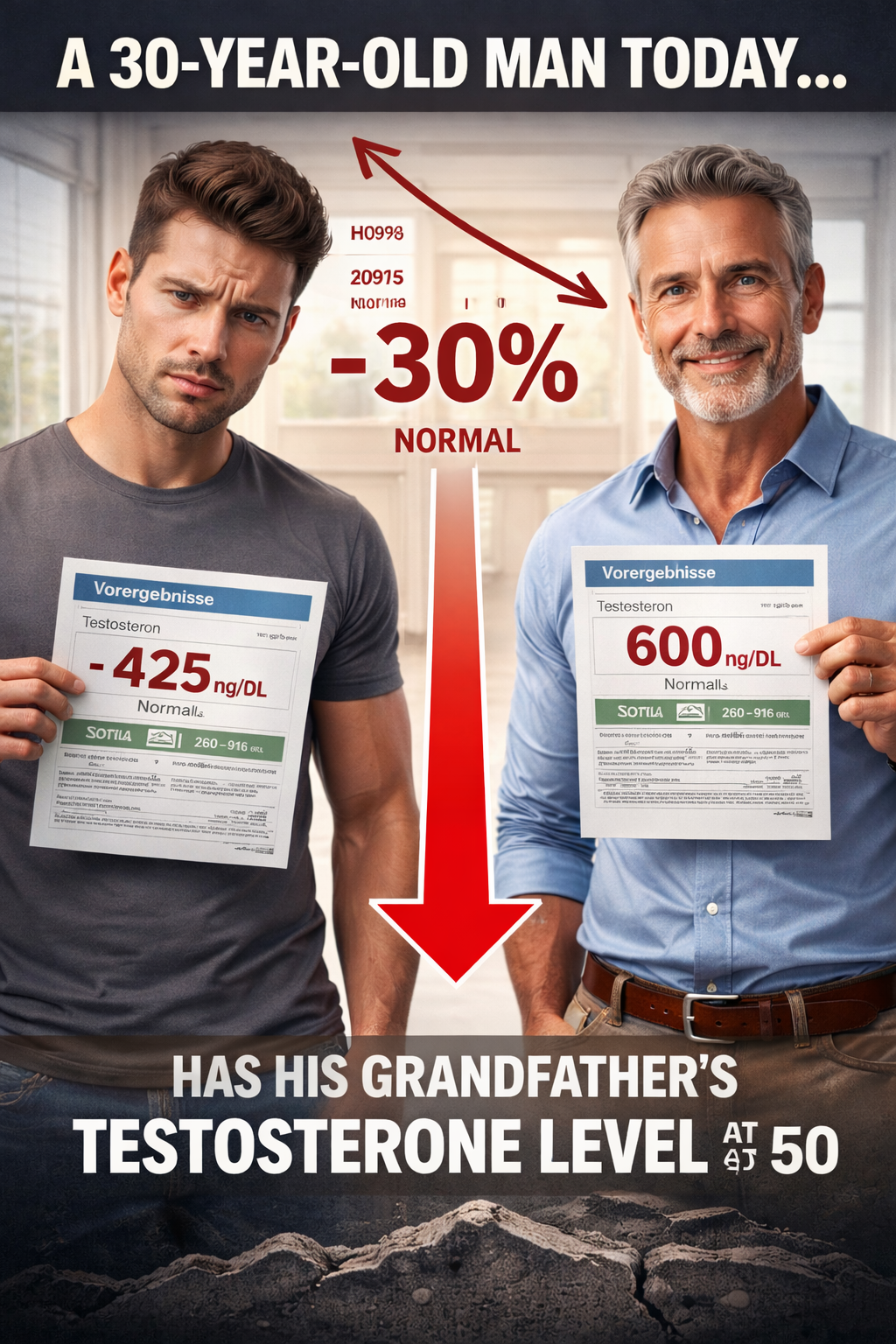
The Silent Collapse: Why a 30-Year-Old Man Today Has His Grandfather's Testosterone Level at 50 And Why Your Lab Report Won't Tell You
There's a health crisis hiding in plain sight. A 30-year-old man today has testosterone levels that would have been considered clinically low in his grandfather's generation. But when he gets his labs checked, he's told everything is "normal."
How is this possible?
Because the reference ranges—the numbers used to determine if you're healthy—have been quietly adjusted downward as the population declined. The bar dropped. And nobody told you.
This isn't speculation. It's published research. And the implications—for individual men, for families, and for our society—are staggering.
The Data: A Generational Collapse
The Numbers Don't Lie
The Massachusetts Male Aging Study established that testosterone levels peak around age 30, then decline approximately 1-2% per year with normal aging. But something else is happening—something beyond normal aging.
Published research from the National Health and Nutrition Examination Survey (NHANES) reveals:
1999-2000: Average testosterone in men ages 15-39 was 605 ng/dL
2015-2016: Average dropped to 424-451 ng/dL
That's a 25-30% decline in just 16 years. The decline occurred even in men with normal BMI. Obesity alone doesn't explain it. Another landmark study—the Massachusetts Male Aging Study—found an age-independent decline of approximately 1.2% per year. This means a 45-year-old man in 2004 had significantly lower testosterone than a 45-year-old man in 1987, despite being the same age.
A 2020 Israeli study of over 100,000 men confirmed: There was a "highly significant age-independent decline in total testosterone in the first and second decades of the twenty-first century." The researchers' conclusion? This decline "does not appear to be attributable to observed changes in explanatory factors, including health and lifestyle changes such as smoking and obesity."
What This Actually Means
Let's make this concrete. Your grandfather at age 50 (circa 1985): Likely had testosterone around 500-600 ng/dL, considered solidly normal for his age. You at age 30 (today): May have testosterone around 400-450 ng/dL—and be told you're "normal" because the reference range shifted. The math: You have LESS testosterone at 30 than your grandfather had at 50. But your lab report says you're fine. Why? Because labs use population-based reference ranges. As the population declined, the "normal" range declined with it. You're being compared to a sinking ship—and told you're floating.
The Reference Range Problem - How "Normal" Gets Redefined
Here's how laboratory reference ranges work: Labs collect data from people who get tested. They calculate the statistical middle 95%. That becomes "normal."
The problem? The people getting tested are:
Predominantly those whose doctors suspect something is wrong
Part of a population with declining testosterone
Often already symptomatic
So the "normal" range includes many men who are already suboptimal. As testosterone levels fall across the population, the range shifts downward to accommodate them. In the 1980s: A testosterone level of 350 ng/dL would have been flagged as LOW. Today: Many labs consider anything above 250-300 ng/dL as "normal." The threshold dropped because the population dropped.
The TSH Parallel
This isn't unique to testosterone. Consider thyroid testing: The "normal" TSH range extends up to 4.5 mIU/L in most labs. But research suggests that up to 30% of people with TSH above 3.0 have undiagnosed autoimmune thyroid disease. The National Academy of Clinical Biochemistry has suggested the true normal range should be 0.4-2.5 mIU/L—nearly half the width of standard ranges. How many people are told they're "normal" while experiencing fatigue, weight gain, and brain fog? The same phenomenon is happening with testosterone—just with far less public awareness.
The Health Consequences of Low Testosterone
This isn't about vanity or gym performance. Low testosterone has serious, documented health consequences.
Cardiovascular Risk and Mortality
A meta-analysis of 37 observational studies with over 40,000 participants found that men with low endogenous testosterone had:
17% increased cardiovascular morbidity
54% increased cardiovascular mortality
A prospective study by Laughlin et al. found that men in the lowest quartile of testosterone had a 40% increased likelihood of 20-year mortality compared to men with higher levels—even after adjusting for other risk factors. A study of 930 men with documented coronary artery disease found mortality was 21% in hypogonadal men versus 12% in men with normal testosterone—nearly double.
Metabolic Health
Low testosterone is associated with:
Increased fat mass, particularly visceral (abdominal) fat
Decreased lean muscle mass
Insulin resistance and increased diabetes risk
Metabolic syndrome
This creates a vicious cycle: low testosterone promotes obesity, and obesity further suppresses testosterone.
Mental Health
The research is striking:
Depressive symptoms have been reported in 35-50% of men with hypogonadism
Low testosterone affects dopamine, serotonin, and GABA—key neurotransmitters for mood regulation
Symptoms include depression, anxiety, irritability, cognitive impairment, and poor concentration
A study published in the Journal of Clinical Endocrinology & Metabolism found that testosterone replacement therapy improved depression scores and cognitive function in men with testosterone deficiency. Cleveland Clinic notes: "When we say people are depressed, what are we describing? We're often describing someone as having low energy and no desire to partake in activities that normally bring them pleasure—these are common things we see with low testosterone, too." How many men are being prescribed antidepressants when the underlying issue is hormonal?
Sexual Function and Fertility
This is perhaps the most obvious consequence:
Decreased libido
Erectile dysfunction
Reduced sperm production and quality
And here's the alarming parallel: Sperm counts have declined over 50% globally since 1973, with the rate of decline accelerating in recent decades. The WHO has had to lower the "normal" sperm count threshold multiple times to keep pace with the declining population.
Bone and Muscle Health
Testosterone is critical for:
Bone mineral density (low T increases osteoporosis risk)
Muscle mass and strength
Physical function and mobility
As men decline earlier, the downstream effects on aging, independence, and quality of life compound.
Why Is This Happening?
The research points to multiple factors converging—many of which didn't exist in your grandfather's generation.
Endocrine-Disrupting Chemicals (EDCs)
This is perhaps the most significant factor. Phthalates (found in plastics, personal care products, food packaging): A study published in the Journal of Clinical Endocrinology & Metabolism found that boys ages 6-12 with higher phthalate exposure had 24-34% lower testosterone levels. In men and women ages 40-60, increased phthalate exposure was associated with 10.8-24% decline in testosterone.
Bisphenol A (BPA) (found in plastics, food containers, receipts):
Detected in urine samples of over 90% of people in the US, Germany, and Canada
Acts as a synthetic estrogen, disrupting hormonal balance
Animal studies show up to 40% reductions in serum testosterone from phthalate exposure
The Endocrine Society stated: "Our results support the hypothesis that environmental exposure to endocrine-disrupting chemicals such as phthalates could be contributing to the trend of declining testosterone and related disorders." These chemicals didn't exist in significant quantities until the 1950s. Your grandfather wasn't exposed to them during critical developmental windows. You were—potentially even in the womb.
Other Contributing Factors
1. Obesity epidemic: Adipose tissue converts testosterone to estrogen
2. Sedentary lifestyle: Physical activity stimulates testosterone production
3. Chronic stress: Elevated cortisol suppresses testosterone
4. Sleep disruption: Testosterone production peaks during sleep
5. Processed food diet: Nutrient deficiencies affect hormone synthesis
6. Microplastics: Now found in human testes and bloodstream
The Transgenerational Effect
Perhaps most disturbing: Research suggests EDC exposure may cause transgenerational effects—meaning your exposure could affect your children and grandchildren's hormone levels, even if they're never directly exposed. Studies in animals have shown decreased testosterone levels in the F3 generation (great-grandchildren) following ancestral EDC exposure. We may be seeing the accumulated effects of three generations of chemical exposure.
The Population-Level Implications
This isn't just about individual men feeling tired. Consider the broader picture:
Fertility Crisis
1. Sperm counts down 52% globally since 1973
2. Rate of decline is accelerating—doubling in speed since 2000
3. Fertility rates dropping across developed nations
4. IVF rates increasing as natural conception becomes harder
Mental Health Epidemic
1. Depression and anxiety rates climbing, particularly in men
2. "Deaths of despair" (suicide, overdose) rising in middle-aged men
3. How much is undiagnosed hormonal dysfunction?
Healthcare Burden
Cardiovascular disease remains the leading killer. Diabetes and metabolic syndrome reaching epidemic levels, Many men are being treated for symptoms while the hormonal root cause goes unaddressed.
Economic Impact
Lost productivity from fatigue, cognitive dysfunction, depression is occurring in alarming numbers. Healthcare costs from downstream metabolic diseases are increasing at an astronomical rate. Fertility treatment costs are increasing as natural conception declines.
What Should "Normal" Actually Be?
This is the critical question. Population-based "normal" (what most labs use):
Lower limit: Often 250-300 ng/dL
Based on the statistical middle of a declining, often symptomatic population
Optimal levels (based on function and health outcomes):
Many researchers and clinicians suggest 500-700 ng/dL for younger men
Based on levels where symptoms resolve and health markers improve
Closer to what healthy men had in previous generations
The difference between "normal" and "optimal" may be the difference between surviving and thriving.
What This Means for You
If you're a man experiencing:
Unexplained fatigue
Loss of motivation
Decreased libido
Difficulty building or maintaining muscle
Increased body fat, especially around the midsection
Brain fog or difficulty concentrating
Mood changes, irritability, or depression
Sleep disturbances
And your labs come back "normal"—don't stop there.
Questions to ask:
1. What is my actual testosterone level, not just whether it's "in range"?
2. What were the reference ranges 20-30 years ago?
3. Am I being compared to a healthy population or a declining one?
4. What would OPTIMAL look like for someone my age?
Consider testing:
1. Total testosterone (standard, but incomplete picture)
2. Free testosterone (the bioavailable portion)
3. SHBG (sex hormone-binding globulin—affects how much testosterone is available)
4. LH and FSH (pituitary hormones that signal testosterone production)
5. Estradiol (elevated estrogen can suppress testosterone effects)
The Bigger Picture
We're living through an unprecedented experiment. In three generations, we've introduced thousands of synthetic chemicals into our environment, food, water, and bodies. We've changed how we eat, sleep, move, and live. The results are measurable: Men today have roughly half the testosterone and sperm count of their grandfathers.
But instead of addressing root causes, the medical system has:
Lowered reference ranges to "normalize" the decline
Treated symptoms with pharmaceuticals
Told men they're "fine" based on adjusted standards
Ignored subclinical dysfunction until disease develops
This isn't healthcare. It's managed decline disguised as normalcy.
A Different Approach
What if we stopped accepting declining standards as "normal"?
What if we:
1. Used optimal reference ranges based on health outcomes, not population statistics
2. Tested comprehensively—genetics, hormones, metabolic function
3. Addressed root causes—environmental exposures, nutrient deficiencies, lifestyle factors
4. Tracked individuals against their own baseline, not shifting population averages
5. Intervened before symptoms became disease
This is the foundation of precision medicine. It's not about comparing you to a sick population and calling you "average." It's about understanding what YOUR body needs to function optimally.
The Bottom Line
A 30-year-old man today has the testosterone of his 50-year-old grandfather. His lab says "normal." His body says otherwise. The reference ranges moved. The bar dropped. And an entire generation of men are being told they're fine while their hormones—and their health—collapse beneath them. Normal is not optimal. Average is not healthy. And decline is not inevitable.
You deserve to know the truth about your biology. And you deserve better than being compared to a declining population and told you're "fine."
References:
1. Travison TG, et al. "A population-level decline in serum testosterone levels in American men." J Clin Endocrinol Metab. 2007;92(1):196-202.
2. Lokeshwar SD, et al. "Decline in Serum Testosterone Levels Among Adolescent and Young Adult Men in the USA." Eur Urol Focus. 2021;7(4):886-889.
3. Chodick G, et al. "Secular trends in testosterone—findings from a large state-mandate care provider." Reprod Biol Endocrinol. 2020;18:19.
4. Laughlin GA, et al. "Low serum testosterone and mortality in older men." J Clin Endocrinol Metab. 2008;93(1):68-75.
5. Corona G, et al. "Hypogonadism as a risk factor for cardiovascular mortality in men: a meta-analytic study." Eur J Endocrinol. 2011;165(5):687-701.
6. Malkin CJ, et al. "Low serum testosterone and increased mortality in men with coronary heart disease." Heart. 2010;96(22):1821-1825.
7. Meeker JD, et al. "Urinary phthalate metabolites in relation to serum anti-Müllerian hormone and inhibin B concentrations." J Clin Endocrinol Metab. 2014;99(9):E1806-E1815.
8. Endocrine Society. "Reduced testosterone tied to endocrine-disrupting chemical exposure." 2014.
9. Swan SH, et al. "The question of declining sperm density revisited." Environ Health Perspect. 1997;105(10):1228-1232.
10. Levine H, et al. "Temporal trends in sperm count: a systematic review and meta-regression analysis." Hum Reprod Update. 2023;29(2):157-176.
11. de Silva N, et al. "Cardiovascular disease and testosterone therapy in male hypogonadism." Ann N Y Acad Sci. 2024.
12. Hudson J, et al. "Adverse cardiovascular events and mortality in men during testosterone treatment." Lancet Healthy Longev. 2022;3(6):e381-e393.